‘Invisibility cloak’ for chemo: Lung cancer treated with one-fiftieth of usual dose
Researchers have found a way to treat drug-resistant lung cancer by packaging a chemotherapy drug in containers made from a patient's own immune system and delivering it directly to tumors. The technique results in 50 times less chemo for patients.
The containers, which protect the drug paclitaxel from being destroyed by a patient's immune system, ensure that the entire dose is delivered to the targeted area.
When administered in the traditional way, paclitaxel is attacked by the body's defenses, which means patients must receive larger doses. This often results in complications such as joint pain, diarrhea, and an impaired ability to fend off actual infections.
Researchers from the University of North Carolina at Chapel Hill came up with the idea of using natural 'delivery containers' while experimenting with exosomes – tiny bubbles derived from the body's white blood cells which are made from the same material as cell membranes and help protect against infection.
"Exosomes are engineered by nature to be the perfect delivery vehicles," Dr. Elena Batrakova, an associate professor at the UNC Eshelman School of Pharmacy, said in a statement. "By using exosomes from white blood cells, we wrap the medicine in an invisibility cloak that hides it from the immune system. We don't know exactly how they do it, but the exosomes swarm the cancer cells, completely bypassing any drug resistance they may have and delivering their payload."
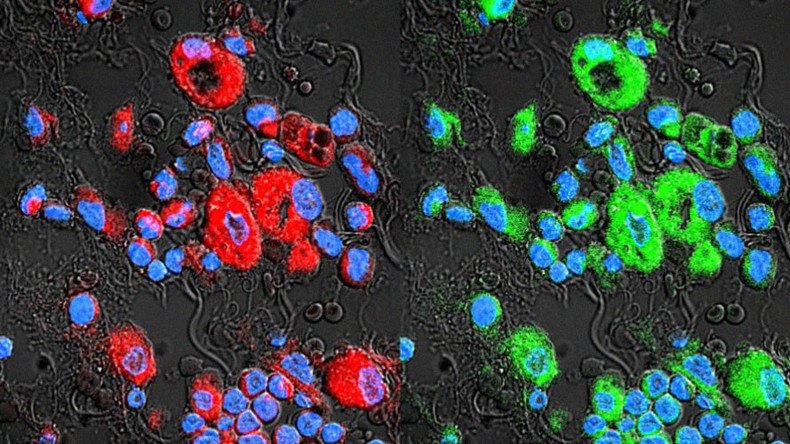
To test the idea, the team used exosomes taken from mouse white blood cells, loaded them with paclitaxel, and pitted them against drug-resistant cancer cells in petri dishes. They discovered that by using the treatment – which they call exoPXT – they could achieve the same level of success with just a fraction of the commonly used dosage.
“...We can use 50 times less of the drug and still get the same results," Batrakova said.
The research, published in the journal Nanomedicine, then went further, testing the therapy in mouse models of drug-resistant lung cancer. The researchers loaded the exosomes with a dye in order to track their progress through the lungs and found they were thorough in seeking out and marking cancer cells.
"Accurately mapping the extent of tumors in the lungs is one of the biggest challenges in treating lung-cancer patients," said Batrakova. "Our results show how powerful exosomes can be as both a therapeutic and a diagnostic."
The finding is a huge step forward for scientists who have been trying for years to find a better way to deliver chemotherapy drugs. Previous techniques have involved plastics-based nanoparticles to package the drugs. These have proved inefficient, however, because the body recognizes the items as foreign and therefore attacks them.














