Superbug scenario: Antibiotic resistance will be ‘catastrophe’ on par with terrorism

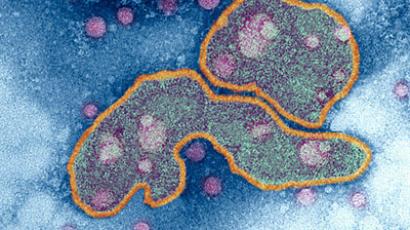
Antibiotic-resistant superbugs will push medical science back to the 19th century, with people dying of minor infections says Britain’s top health official.
Dame Sally Davies, chief medical officer for England, said action is urgently needed to fight antibiotic and antimicrobial resistance and that new drugs must be developed to treat new mutating infections.
She warned that if nothing is done to reverse the situation Britain would face an apocalyptic scenario with “a health system not dissimilar from the 19th century.”
Two months ago Dame Davies warned British legislators that antibiotic resistance should be added to the UK’s national risk register. The register was set up in 2008 to advise the public and businesses on national emergencies that the UK could face in the next five years.
The highest risks currently on the list include a catastrophic terrorist attack, a flu pandemic and coastal flooding, as was seen during the 1952 North Sea flood, the last time a national emergency was called in the UK.
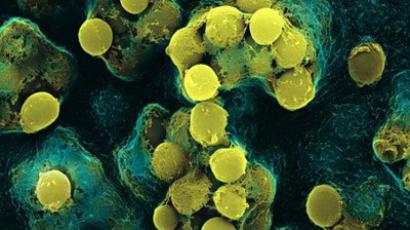
As bacterial infections evolve into ‘superbugs’ like MRSA, which are resistant to existing drugs, more must be done discover new antibiotics. Only a few antibiotics have been discovered in the last few decades.
“Antimicrobial resistance poses a catastrophic threat. If we don’t act now any one of us could go into hospital in 20 years for minor surgery and die because of an ordinary infection that can’t be treated by antibiotics, And routine operations like hip replacements or organ transplants could be deadly because of the risk of infection,” Davies told reporters as she published her report on infectious disease.
Untreatable superbugs are popping up all over the world. A superbug with a mutation known as NDM 1, which was first detected in India, has now turned up in most other countries. There have also been cases of a totally drug-resistant form of tuberculosis and the World Health Organization (WHO) said an untreatable form of gonorrhea was spreading round the world.
MRSA, one of the best known superbugs, is estimated to kill 19,000 people every year in the US and a similar number in Europe, far more than HIV and AIDS.
Davies’s research has been welcomed by scientists and medical professionals.
“There are an increasing number of infections for which there are virtually no therapeutic options. And we desperately need new discovery, research and development,” Laura Piddock, professor of microbiology at Birmingham University and director of Antibiotic Action, a campaign group, told Reuters.
Davies has called for better cooperation between the pharmaceutical and healthcare industries in order to focus on developing new antibiotics as well as preserving the arsenal of existing ones.
She also called on governments to take the threat seriously and suggested the WHO and the G8 encourage more innovation in the field of antibiotics.
“Over the past two decades there has been a discovery void around antibiotics, meaning diseases have evolved faster than the drugs to treat them,” said Davies.
Although a small number of new individual drugs are being developed, no new classes of antibiotics have been developed since 1987. The main reason, explains Davies, is that is there little money to be made in developing new courses of antibiotics.
She added that more effort should be made by doctors to prescribe antibiotics only when needed and that hygiene should be improved in hospitals to make sure infections were kept to a minimum.
Keith Ridge, the UK government’s chief pharmaceutical officer, said that although the number of antibiotics prescribed in hospital had fallen, there still needed to be tighter control of antibiotic prescriptions in GP’s surgeries.
“We need new ways to kill resistant bacteria or reduce their carriage of resistant genes. Novel approaches that might have appeared unrealistic a few years ago need to be explored,” Professor Christopher Thomas, professor of molecular genetics at the University of Birmingham, told the Independent.
The WHO made drug resistance the focus of its 2011 World Health Day, warning the
“world is headingtowards a post-antibiotic era, in which many common infections will no longer have a cure and, once again, kill unabated.”