Killer strain: TDR tuberculosis strikes India
A strain of “totally drug-resistant” tuberculosis has come to light in India. So far, the virtually untreatable form of the lung disease, which has a mortality rate of over 50 per cent, has infected at least 12 people.
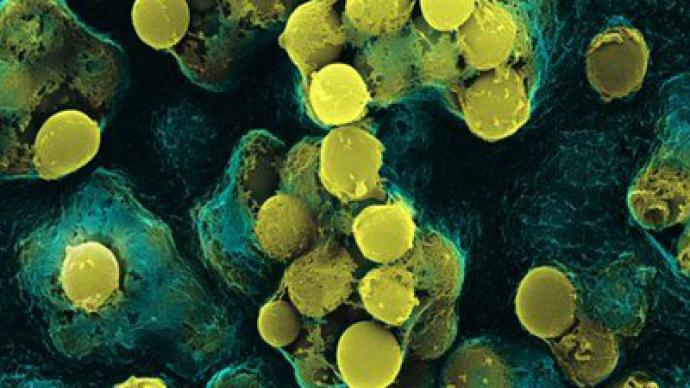
Physicians in Mumbai are calling the new strain TDR, for Totally Drug-Resistant tuberculosis. TDR has been isolated in the fluid samples of 12 tuberculosis patients in the past three months at Hinduja Hospital alone, the Indian Times reported.The patients, including a 13-year-old girl, were diagnosed in October. One of the 12 infected patients, a 31-year-old woman, died in November 2011.A day after doctors at Hinduja Hospital published their study of 12 TDR patients, a team of state health department and civic officials got in touch with them to deal with the issue. “Coordination between the private and public sector is the way forward to improve the situation,” said Dr Zarir Udwadia, a consultant physician at the hospital.Last Friday, the joint director for tuberculosis at the state health department, Dr PY Gaikwad, played down the Hinduja hospital findings, saying they were not valid as the hospital’s laboratory was not accredited to detect such cases.However, according to Dr Udwadia, the Hinduja hospital's laboratory is recognized by the World Health Organization and “most government centers send their sputum samples to Hinduja hospital’s microbiology laboratory for drug sensitivity tests.”The public health community is familiar with other cases of highly-resistant strains of tuberculosis and largely accepts that there could be many more which have gone undocumented.
The term TDR has not been clearly defined for tuberculosis. While the concept of TDR is easily understood in general terms, in practice, in vitro drug susceptibility testing (DST) is technically challenging and limitations remain on the use of results. New drugs are being developed, and their effectiveness against these TDR strains has not yet been reported. For these reasons, the term TDR tuberculosis is not yet recognized by the WHO. For now, these cases are defined as extensively drug-resistant tuberculosis (XDR-TB), according to WHO definitions. TB bacilli with different levels of resistance spread in the same way and with the same risk of infection as fully drug-susceptible strains. WHO is organizing an Expert Group Meeting in March 2012 to assess additional data on DST accuracy obtained since 2008. This meeting will be expanded to include a consultation on possible definitions for “totally drug-resistant” TB.
The two earliest recorded cases of TDR tuberculosis were in Italy in 1995 and 1998. The scientific journal Eurosurveillance, which specializes in epidemiology, published a study about the two strikingly similar Italian cases which both proved resistant to drug treatment. In both cases, the patients were young females from middle-class families who were treated for eight and five years with 17 different antibiotics. Despite protracted treatment, they both died in 2003. In 2009, doctors registered 15 cases of TDR tuberculosis in Iran, mostly in deprived areas. In that outbreak, the contagion did not spread widely either.Tuberculosis is mainly transmitted through close personal contact and is far less contagious than the flu. Therefore it is unlikely that the TDR strain will spread rapidly and cause an epidemic.Even without a TDR strain, tuberculosis is still one of the deadliest diseases in the world. In 2009, the world saw over 1.7 million deaths from various forms of tuberculosis. In its active form, tuberculosis has a death rate of over 50 per cent if untreated. Its treatment is difficult and requires a 6-12 month course of antibiotics. If the course is interrupted, the disease mutates and develops resistance to a particular drug, making the further treatment less effective. The official opinion on TDR is that these cases are in fact mutations created by poor or insufficient drug treatment. The Eurosurveillance study confirms that, saying that “in both [Italian] cases the drug susceptibility tests showed that resistance to new drugs was acquired over time.”














