Don’t get surgery at the end of the week: UK hospital weekend death spike

Patients undergoing planned operations in NHS hospitals towards the end of the week, increase the risk of death, according to a groundbreaking new study published in the British Medical Journal on Tuesday.
The subject group contained over 4 million participants who
underwent different procedures between 2008 and 2011.
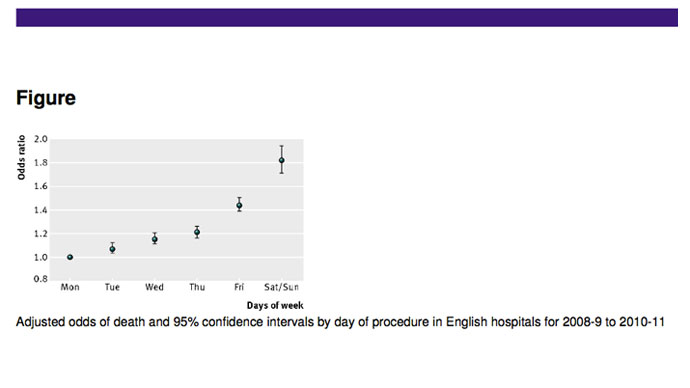
Patients who had surgery on a Friday were found to be 44 per cent
more likely to die than those who had operations at the beginning
on the week – the risk of death increased incrementally as the
week progressed.
Weekend death rates were a staggering 82 percent higher than on a
Monday. However, the study also noted that number of patients
undergoing surgery on weekends was considerably smaller.
“Death rates were lowest for patients having operations on
Monday, increasing by around 10 per cent for each subsequent day
of the week,” stated the study, called “Day of week of
procedure and 30 day mortality for elective surgery:
retrospective analysis of hospital episode statistics,” which
was undertaken by the School of Public Health at Imperial College
London.
Researchers drew conclusions by linking hospital administrative
data with death certificates, using records from 163 trusts and
records containing basic information such as age, sex, and source
of admission, alongside other variables such as area level of
socioeconomic deprivation based on the postcode of a patient’s
residence.
The study’s authors suggested that the root of the problem may
have been have been related to the lower quality of staff working
at the weekends combined with a stronger reliance on temporary
workers on non-traditional working days.
It said that the first 48 hours following surgery were critical.
However, researchers stated that the study monitored the death
rates of patients after discharge too, to get a more accurate
impression.
Its researchers claimed that previously, no “large nationally
representative studies have examined the day of elective
procedure while also accounting for deaths after discharge.”
Because the first 48 hours are so vital, if the quality of care
is lower at the weekend as some previous studies have suggested,
“we would expect to see higher mortality rates not just for
patients operated on at the weekend, but also those who have
operations towards the end of the week, whose postoperative care
overlaps with the weekend,” said Dr Paul Aylin, who led the
study.
Critics stated that the statistics were of great cause for
concern and said discrepancies were ‘unacceptable.’
“The NHS still seems to work 9am to 6pm Monday to Friday when
it needs to be responding to the needs of patients and the
public,” Katherine Murphy, chief executive of the Patients
Association told the Telegraph.
An ongoing investigation is currently examining 14 NHS hospitals
with unusually high death rates, to see whether staff shortages
were a factor, Professor Sir Bruce Keogh, NHS England medical
director, added in the article.
It had been recognized in the study’s introduction that “a
substantial number of patients die as a result of unsafe medical
practices and care during their admission to hospital.”
However, a thorough examination of the reasons that may have been
behind this had never thoroughly been given, and it was thought
that surgery carried out at weekends carried higher risks.
“Some research has proposed reduced staffing levels or less
senior and less experienced staff at the weekends as an
explanation, and there is evidence to support the staffing
hypothesis,” the study said.
Its findings suggested a potentially much stronger “’weekday’
and ‘weekend’ effect” for elective procedures than is seen in
emergency admissions, also finding some similarities depending
upon procedure type.
Several “specific high risk procedures,” were monitored
and the same trend was found for higher mortality close to the
weekend.














