Drug-resistant bacteria: 23,000 deaths a year in US and getting worse

A lack of new antibiotics, coupled with the over-prescription of existing ones, is making many formerly routine diseases untreatable, according to a new report published by the US Centers for Disease Control and Prevention (CDC).
At least two million people in the US are infected each year - and 23,000 of those die - from bacteria that does not respond to treatment by usual or any antibiotics, claims the Antibiotic Resistance Threats in the United States 2013 report.
“We are approaching a cliff. If we don’t take steps to slow or
stop drug resistance, we will fall back to a time when simple
infections killed people,” said Michael Bell, Deputy Director
of CDC’s Division of Healthcare Quality Promotion, and one of the
report’s authors.
Among the diseases the report labeled an ‘Urgent threat’ are
C.difficile, a form of severe diarrhea that kills 14,000 people
per year, and gonorrhea, as nearly a third of the 800,000
estimated annual infections are with strains that do not respond
to at least some antibiotics.
The most terrifying perhaps is Carbapenem-resistant
Enterobacteriaceae (CRE), a relatively new and rare but deadly
infection that cannot be tackled by “drugs of last resort”
(medicines that are purposely reserved for treatment courses when
all else has failed).
Out of an estimated 9,000 cases of CRE each year, 600 people die.
The report says that by far the most important reason for the
proliferation of drug-resistant bacteria is the incorrect
prescription of antibiotics by doctors and improper use by
patients.
Half of all antibiotic prescriptions in the US are unnecessary –
a precaution, or a result of misdiagnosis or ignorance about the
ability of the drug to treat a certain disease. A course of a
drug weeds out certain types of bacteria, but leaves a minority
untouched. The surviving bacteria then multiply, creating a new
strain of the disease that is no longer susceptible to that
medicine. The problem is made worse when patients stop their
antibiotics course too early – often as soon as they feel better
– as the remaining microorganisms then have a better chance of
escaping.
“Every time antibiotics are used in any setting, bacteria
evolve by developing resistance and that process can happen with
alarming speed. These drugs are a precious, limited
resource—the more we use antibiotics today, the less likely we
are to have effective antibiotics tomorrow,” said Steve
Solomon, Director of the CDC’s Office of Antimicrobial
Resistance.
Another breeding ground for superbugs is livestock farms – the
destination of up to 80 percent of all antibiotics - where
animals are routinely prescribed drugs, mostly as a preventative
measure and to make sure they grow as large as possible. The
strains produced in those circumstances are then passed on to
humans, creating additional danger.
Estimating the exact number of people who have been infected and
died from a drug-resistant bacteria is by nature an imprecise
activity.
But the authors say they are not scaremongering.
“This is a bare minimum, a very conservative estimate,” said
CDC Director Thomas R. Friedman, noting that the authors have
tried to separate cases when the drug-resistant infection was
directly responsible for death, as opposed to a contributing
factor.
“The actual number of infections and the actual number of
deaths are certainly higher,” states the report.
One of the problems of drug-resistance is the relative scarcity
of new antibiotics. Until the current ones stop working in
sufficient numbers, pharmaceutical companies have little
incentive to develop them for currently curable diseases. The
report urges the government to invest more money in antibiotics
as a matter of national importance, though several programs are
already in place.
But even if US doctors and companies take every measure
available, there is only so much they can do in a globalized
world.
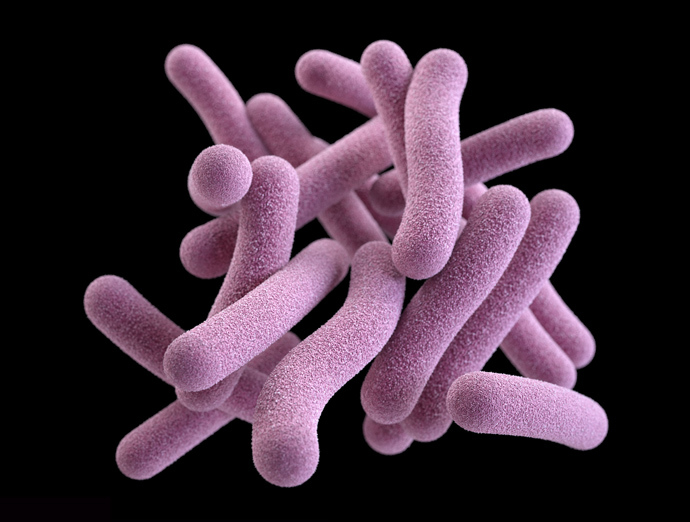
In countries such as China and Russia, where antibiotics are
freely available over-the-counter and are consumed by an order of
magnitude more often than in the United States, drug-resistant
strains are emerging at a much faster rate (and involve diseases
like tuberculosis that are already more deadly). And these
strains are sure to spread throughout the globe.
"We're facing a catastrophe," said Helen Boucher, a Tufts
University expert and spokeswoman for the Infectious Diseases
Society of America.