‘Devastating’ implications of drug-resistant superbugs now a reality – WHO

Deadly antibiotic-resistant superbugs are a ‘serious threat’ to world health and no longer merely a prediction for the future, according to a new report by the World Health Organization (WHO). Previously treatable illnesses can now once again kill.
“The world is headed for a post-antibiotic era, in which common infections and minor injuries which have been treatable for decades can once again kill,” said Keiji Fukuda, the WHO's assistant director-general for health security.
The new resistance has the capacity to strike anyone, of any age, on a global scale according to the WHO report, entitled ‘Antimicrobial resistance: global report on surveillance’, released on Wednesday. It’s the organization’s first ever global report on antibiotic resistance.
“The implications will be devastating,” stated Fukuda.
Data spanning 114 different countries was utilized in the study and superbug resistance was found in all regions of the world. The infections were even resistant to a class of antibiotic which fall into a category known as carbapenems – a broad-spectrum beta-lactam antibiotic considered one of the last resorts in the treatment of infectious bacterial diseases.
Resistance to last-resort treatments for potentially deadly hospital infections caused by the common Klebsiella pneumoniae bacteria have been found in all parts of the world, as has resistance to the most common drugs to treat urinary tract infections caused by E.coli, as well as last resort gonorrhea treatment in 10 developed countries – among them the UK.
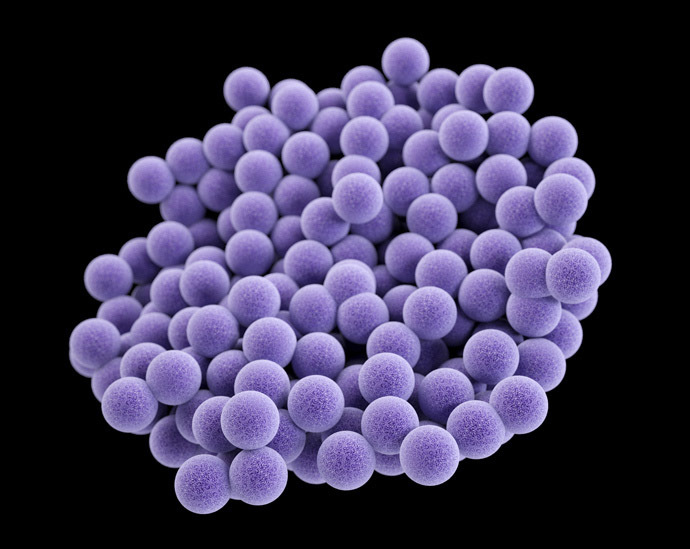
One of the best knows superbugs is MRSA – a staph infection – which is estimated to kill some 19,000 people every year in the US and an equal number in Europe. A new study released last week showed that MRSA, commonly found in hospitals, has settled in a new stronghold – that is US homes, which are a “major reservoir” of a strain called USA300.
Experts have suggested that the resistance of superbugs stems from the overuse or misuse of antibiotics and “threatens the achievements of modern medicine.”
Antibiotic resistance is when bacteria adapt and change so that antibiotics no longer work in the treatment of the diseases.

While it has been a prominent 21st century public health concern, the worries have previously remained confined to the realm of predictions rather than actual commentary on present conditions. Resistance was nil when drugs were first introduced to combat such diseases in the 1980s. However, there are now countries where drugs have no impact whatsoever in more than half of all patients.
“Unless we take significant actions to improve efforts to prevent infections and also change how we produce, prescribe and use antibiotics, the world will lose more and more of these global public health goods and the implications will be devastating,” Fukuda said.
In response to the WHO report, campaign group Antibiotic Action
“specifically” called for steps to be taken.
They called for the “establishment of a fully funded global
mandatory surveillance program and global/region specific action
plans to monitor and contain antimicrobial resistance,”
along with advocating strategies to counter the broad global
availability of antibiotics.
“The world needs to respond as it did to the AIDS crisis of the 1980s. To do this, we need to be ambitious to succeed – moves such as a fully funded mandatory global surveillance program will document the size of the problem and funded public education will help minimize use – but these are just starting points,” Laura Piddock, director of the group stated.














