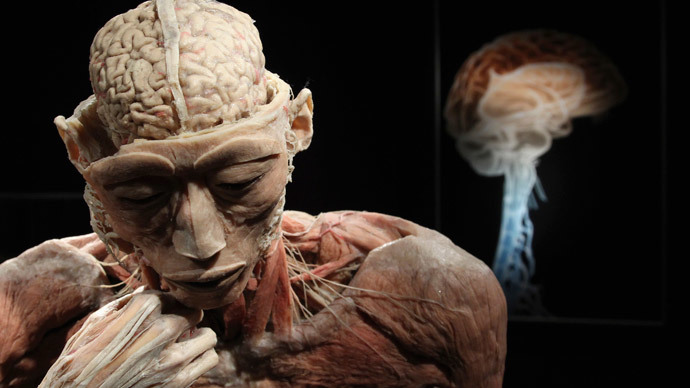
Depression makes your brain smaller – study

Persistent depression shrinks the human brain’s center responsible for emotions and memory that might lead to changes in a person’s behavior and even losing their identity, a global interdisciplinary study has revealed.
A new global study has finally proven that brain damage is a consequence of repeated depression instead of being its prerequisite or a predisposing factor. This conclusion draws the final line under the decades of unconfirmed hypothesizing.
Some shrinkage of the brain has long been connected to depression, although without clear evidence, as variances in types of depression, treatment methods as well as a small sample size have led to inconsistent results.
Now, the largest international survey, which brought together the efforts of 15 research institutes from the US, UK and Australia and allowed scientists to combine the results of their smaller studies, revealed that recurrent depression shrinks the hippocampus – the so-called emotional center of the brain, which is a part of the brain’s limbic system.
“This study confirms – in a very large sample – a finding that’s been reported on quite a few occasions – the fact that the hippocampus is particularly vulnerable to depression,” said Philip Mitchell, scientia professor & head of the School of Psychiatry at University of South New Wales, Australia, who took part in the research.
READ MORE: Russian scientists find new way to repair DNA that may cure Alzheimer’s
Apart from forming emotions, the hippocampus is also responsible for forming new memories and connecting emotions to those memories as well as is involved in long-term memory processes.
While the hippocampus plays such an important role in the brain’s functioning, its damage could engender serious consequences.
“Your whole sense of self depends on continuously understanding who you are in the world – your state of memory is not about just knowing how to do Sudoku or remembering your password – it’s the whole concept we hold of ourselves,” said professor Ian Hickie, from the University of Sydney’s brain and mind research institute, who led the Australian arm of the study.
“When you shrink the hippocampus, you don’t just change memory, you change all sorts of other behaviors associated with that – so shrinkage is associated with a loss of function,” he adds.
READ MORE: Trusting the app: Blind French hikers use new technology to cross mountains
The cooperation of 15 research institutes allowed the scientists to conduct a cross-sectional analysis of 9,000 people’s brain scans.
The research team used magnetic resonance imaged (MRI) brain scans and clinical data from 1,728 people with major depression and 7,199 healthy individuals, combining 15 datasets from Europe, the US and Australia, as well as samples obtained from an international consortium studying psychiatric disorders, the ENIGMA group.
The results of the study were published in Molecular Psychiatry on June 30.
The scientists found that people who had a smaller hippocampus suffered from recurrent episodes of depression or got depressed at an early age (before the age of 21). Such people accounted for 65 percent of the depressed study participants.
Hickie said the study’s findings suggested that chronic depression is what does the damage.
“I think this resolves for good the issue that persistent experiences of depression hurt the brain,” he said.
“Those who have only ever had one episode do not have a smaller hippocampus, so it’s not a predisposing factor but a consequence of the illness state,” he said, adding that “the more episodes of depression a person had, the greater the reduction in hippocampus size.”
READ MORE: Home to extraterrestrials? Philae probe could be sitting on comet filled with alien life
The study’s findings emphasized the importance of the early treatment of depression, especially in teenagers and young adults.
“So recurrent or persistent depression does more harm to the hippocampus the more you leave it untreated,” said Hickie, highlighting that identifying and treating depression as soon as it first occurs was essential to prevent brain damage.
The research also showed that patients taking antidepressants had a larger hippocampus, thus indicating the possible protective effect of those medicines.
“There is a lot of nonsense said about antidepressants that constantly perpetuates the evils of them, but there is a good bit of evidence that they have a protective effect,” said Hickie, although he emphasized that antidepressants “are not the only treatment” as a “broad range of treatments that should be explored” with psychotherapy “explored as the first line of treatment, not medicines.”
READ MORE: Alzheimer's symptoms could appear 18yrs before diagnosis – study
Paul Fitzgerald, professor of psychiatry at Monash University, Melbourne, said that the results of the study had a fundamental scientific value.
“I don’t think there’s anything that’s really, fundamentally going to change overnight – but it’s an important part of the jigsaw puzzle to put together a better understanding of what’s going on in depression,” he said.
Fitzgerald added that researchers would continue the studies by measuring the volumes of individual regions within the hippocampus, as it would “provide greater capacity to draw conclusions.”
The research team also claimed that some evidence indicates that the damage inflicted to the brain by depression could be reversible with the right treatment.
“Other studies have demonstrated reversibility, and the hippocampus is one of the unique areas of the brain that rapidly generates new connections between cells, and what are lost here are connections between cells rather than the cells themselves,” Hickie said.
He also emphasized that “treating depression effectively does not just mean medicines. Social interventions are just as important.”












